Physiotherapy is the “best job in the world!” Or at least that is my opinion (though I suppose I am biased). My experiences as a student physiotherapist have reinforced this opinion for me and affirmed that my decision to pursue a career in physiotherapy is the best decision I have made.
By way of introduction, my name is Dan. Many of you may have met me over the past 4 weeks, but for those of you who don’t know me, I’ll give you a brief summary…
I’ve just completed the final year of my physiotherapy MSc at the University of Birmingham. I have an interest in musculoskeletal physiotherapy and have completed a range of clinical placements, including hospital-based and sports-club based, and have most recently rounded off my experience as a student with my elective placement at Ashbourne and Hilton Physiotherapy.


Charlotte King – our experienced Physiotherapist overseeing & assisting Dan with
physio treatments
At the beginning of my placement, the clinic asked me if I would like to write a Blog for the website and of course, I jumped at the opportunity!! The brief.. to write about anything I wanted to, which also means that what I have written is my opinion and hasn’t been influenced by anyone else.
Probably unsurprisingly, my opinion is that Ashbourne and Hilton Physiotherapy is great. The staff and patients alike are friendly and welcoming, always happy to help, and they are very good at what they do. As a student, I have a few important criteria that I feel make a high-quality placement. Firstly, and probably obviously, is for the staff to be friendly and welcoming. I feel that as a student this allows you to relax and builds your confidence as you progress. Secondly is having a knowledgeable educator who can teach you and challenge you as a student practitioner to progress your skills and learning. Thirdly is working in an environment in which you are trusted to work independently and make your own clinically reasoned decisions.
This was a high-quality placement. The team at Ashbourne and Hilton didn’t just meet these criteria, they massively exceeded them. They created the perfect environment for me to work in, allowing me to manage my own caseload, see my own list of patients and work independently.
As an educator, I could not have asked more of Charlotte. She trusted me from day one to work independently, supported me throughout the placement and advised me when I needed assistance, and taught me a lot, especially things that we are not taught at university. This allowed me to really develop as an independent and autonomous practitioner, and hugely developed my skillset and what I have to offer as a physiotherapist moving forward. Essentially, Charlotte and the team created an environment that mimicked that of a junior physiotherapist working in a musculoskeletal clinic, which is handy given that the next time I work in a physiotherapy clinic, that will be me.
It’s also a really nice place to be. It’s clean, modern and spacious, has a great range of equipment and facilities, and yes, the aircon was priceless when in reached 40 degrees outside. And as a side note, the patients of the clinic are great too. Every single patient I had contact with was lovely and supportive. It must be that northern charm (and yes, this counts as north to me as I grew up a couple of hours south of Derbyshire!). So well done Ashbourne, keep it up.
I loved my time at the clinic and although I was only there for 4 weeks, I learned a huge amount, and feel very ready to step out into the big wide world of being a qualified physio. As much as I could go on and on about my experience at the clinic, I also thought it would be valuable to discuss something slightly more clinical.
One musculoskeletal condition that I encountered numerous times throughout my placement, and something that is of interest to me, is tendinopathy. Tendinopathy (previously referred to as tendonitis or tendinosis) is a pathology (problem) with the tendon (the part of soft tissue that attaches muscles to bones and acts as a ‘pulley system’ to allow us to move) that often results in pain, reduced function, and sometimes swelling, of the tendon (Kaux et al., 2011). It occurs all over the body, but typical areas include rotator cuff tendinopathy in the shoulder, lateral elbow tendinopathy or tennis elbow, patella tendinopathy of the kneecap, and Achilles tendinopathy in the Achilles tendon (Millar et al., 2021).
The symptoms of tendinopathy are typically quite straightforward and tend to involve pain in the affected area of the tendon, that usually increases during activity and eases when resting. Depending on which tendon is affected, some swelling or thickening of the tendon may also be present. The range of movement of the local joint is also often limited (Wilson and Best, 2005).
Tendinopathy has been researched quite substantially over the past few years, and current thinking suggests that whilst on a molecular level it is quite complicated, it is usually as a result of a few factors and phases: reactive, disrepair, and degeneration (Cook and Purdam, 2009).
The first is the reactive phase, which relates overload of the tendon and refers to overstressing the tendon through activity that it is not accustomed to. For example, using the hedge trimmers for the first time of the year, or taking up a sport that you haven’t played since you were in your twenties and slightly over-doing it! Overload can also occur because a tendon hasn’t been used as much as it should be and has become deconditioned, meaning your usual activities can cause the tendon to become aggravated.
Without boring you with too much science, tendons are made up of proteins called collagen and elastin (imagine the individual fibres of a rope) and proteoglycans which hydrate the tendon (Loiacono et al., 2019). These are important because current thinking suggests that when a tendon becomes overloaded and irritated, the proteoglycan and or water content of the tendon increases causing it to become thickened in order to dissipate the load on the tendon. But this can cause some of your pain and isn’t always as helpful it should be!
The second phase is the disrepair phase which is the tendons attempt to heal. This is very similar to what happens in the reactive phase, but in this phase the increase of the water content in the tendon causes collagen and elastin fibres to begin to separate slightly (imagine a rope beginning to fray where the fibres are less tightly wound).
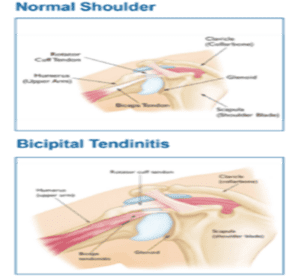
The third and final phase is termed the ‘degenerative’ phase where the tendon becomes quite disordered, and the volume of collagen is heavily reduced (imagine a rope where some of the fibres in the middle have been taken out). This causes the tendon to become quite weak and not very pretty to look at under a microscope. But remember, it is very uncommon to get to this stage.
The good news with tendinopathy is that physiotherapy is very effective. The aims of the treatment are to optimise the loading of the tendon, e.g. advice on which activities to avoid and which activities to carry on with, and to strengthen the tendon and surrounding muscles. There are also a number of other treatments such as massage and electrotherapy that can help to reduce pain and improve the healing process of the tendon. All of this treatment allows us to reverse the phases that are discussed above and return the tendon to being happy and healthy.
The two main types of exercises that are often prescribed for tendinopathy are isometric exercises and eccentric exercises. Isometric exercise refers to an exercise where the muscle is contracting in a fixed position, for example pushing your foot against a wall, and this can be helpful for reducing pain and gently reintroducing load (Rio et al., 2015). Eccentric exercise refers to an exercise where the muscle is contracting as it is being lengthened, for example slowly straightening your elbow whilst holding a weight. This helps to improve the healing process of the tendon to return in to a ‘normal’ state (Chen and Baker, 2020). Below are some examples of the different exercises that you might be prescribed for different tendinopathies.
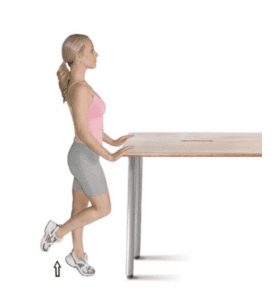
Isometric Calf Raise
Use both feet to raise up onto your toes then take one foot off the floor and hold the position shown.
 Isometric Wall Squat for Patella Tendinopathy
Isometric Wall Squat for Patella Tendinopathy
Open your legs slightly wider than shoulder width, stand with your back resting against a wall, and bend your knees to the 1/2 squat position. Hold the down position. Make sure you keep the middle of your knn-cap in line with the middle toes of your foot. This exercise will help to strengthen your quadticep muscles, knee joints and legs.
Image credit: www.ingeniovirtual.com

Eccentric Posterior Cuff Strengthening Band Hand
Lie on your back on the floor or a bed. Place a few towels under your elbow to bring your shoulder forward slightly. Place your opposite hand on your affected shoulder to prevent the shoulder from raising too much. Loop an exercise band around your foot and wrist on the same side. Keep your knee bent at 90 degrees. Keep your elbow at 90-90. Pull your arm into full external rotation against the resistance of the band. Straighten out your leg sliding it down to the straight position. Control the return movement of your arm back to the 90-90 position. Bend your knee again to take the tension out of the band and to restart the exercise. This will target the posterior rotator cuff to strengthen it eccentrically.
 Eccentric wrist extension with dumbbell for Tennis Elbow
Eccentric wrist extension with dumbbell for Tennis Elbow
Rest your arm on a table with your palm facing down, and hold a 1-2kg dumbbell. Lift your hand upwards using your hand, and then with a controlled movement let the weight pull your hand back down. At the bottom, repeat by lifting your own hand upwards again, and then letting the weight pull your hand back down. Movement down should be slow. Eccentric exercises are a very effective way to rehabilitate the wrist, forearm and elbow, and this can be especially useful for tennis elbow.
Image credit: www.whyexercise.com
Hopefully I haven’t bored you all to sleep with this blog and it’s maybe even been interesting! I won’t waffle on any longer, but just remember, as with tendinopathy, physiotherapy can be an excellent solution a number of musculoskeletal issues and is often the first line treatment for many conditions.
This blog isn’t an advert for the clinic, more a review of my experience in working here as a student on placement, but in my opinion, Ashbourne and Hilton Physiotherapy is a wonderful clinic with a very talented and knowledgeable pool of staff and I can safely say from my experience working with the team that you will be in safe hands at this clinic.
I’d like to thank Lorna, Charlotte and the rest of the team for being so accommodating and helping me to progress my physiotherapy career. I look forward to staying in contact with the clinic and following its progress.
References
Chen, Z., Baker, N.A. (2020). Effectiveness of eccentric strengthening in the treatment of lateral elbow tendinopathy: A systematic review with meta-analysis. J Hand Ther 34, 18–28.
Cook, J.L., Purdam, C.R. (2009). Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. British Journal of Sports Medicine 43, 409–416.
Kaux, J.-F., Forthomme, B., Goff, C.L., et al. (2011) Current Opinions on Tendinopathy. Journal of Sports Science & Medicine, 10 (2): 238–253.
Millar, N.L., Silbernagel, K.G., Thorborg, K., et al. (2021) Tendinopathy. Nature Reviews Disease Primers, 7 (1): 1–21.
Rio, E., Kidgell, D., Purdam, C., et al. (2015) Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. British Journal of Sports Medicine, 49 (19): 1277–1283.
Wilson, J.J. and Best, T.M. (2005) Common overuse tendon problems: A review and recommendations for treatment. American Family Physician, 72 (5): 811–818.
#ashbournephysiotherapy #ashbournephysiotherapy&sportsinjuriescentre #hiltonphysio #hiltonphysiotherapy #students #studentplacement #tendinopathy #achillesinjury #tenniselbow #shoulderinjuries #patella #kneepain #kneeinjruy #ashbourne #hilton